Menu
Call: (647) 352–3233 | (647) 735–4604 | (416) 639–1712 | Fax: (416) 630–6415
ELITE – Laser Hemorrhoidoplasty (old page)
Book Hemorrhoid Removal Consult
Send a Referral Form to your Doctor
What are hemorrhoids?
Hemorrhoids are a natural part of the human body and, when healthy, assist with the closure of the anus.
Hemorrhoids are vascular cushions that move blood to and from the anus and help support the function of the sphincter. Most people think of hemorrhoids as the disorder known as hemorrhoids or piles.
Hemorrhoids as a disorder are swollen veins or blood vessels in and around your lower rectum and anus, similar to varicose veins. These swollen vessels cause irregular protrusions, which can cause pain and bleeding. They are very common for both males and females and will occur in approximately half of the population by age 50.
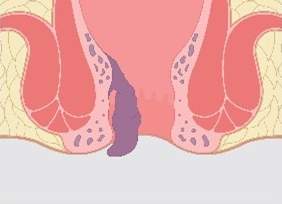
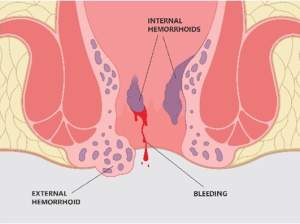 Hemorrhoids can be both internal and external.
Hemorrhoids can be both internal and external.
Internal hemorrhoids either do not protrude out of the anus or return inside either on their own or by manual manipulation.
They are often painless but tend to cause bleeding. External hemorrhoids are located outside of the anus and can often feel like small lumps. They tend to cause discomfort, itching and difficulty sitting.
Symptoms of Hemorrhoids
- Pain during bowel movements
- Blood in stool or toilet bowl
- Itching and/or irritation around the anus
- Pain while sitting
- Tissue swelling around the anus
- Anal discharge
What are the risk factors for hemorrhoids?
- Obesity
- Pregnancy
- Lifting heavy
- Straining on the toilet
- Sitting for long periods
- Family history of hemorrhoids
- Long-term or chronic constipation or diarrhea
What is the ELITE Hemorrhoid Treatment?
The ELITE Hemorrhoid Treatment (Laser Hemorrhoidoplasty) is an innovative treatment option that is minimally invasive option that uses laser to treat hemorrhoids. During this procedure, a laser probe is inserted into the targeted hemorrhoid and activated. In its active state, the laser causes the arterial flow to coagulate, resulting in shrinkage of the hemorrhoid over the next several days.
ELITE does not require any incisions or sutures, which reduces the risk of infection, incontinence and pain significantly.
Advantages:
- Very effective
- Minimal to no pain
- Quick return to normal activities
- Minimally invasive
- Low risk of infection
- No incision or sutures required
- Low to no chance of incontinence
- Can be used on all grades of hemorrhoids
Grades of Hemorrhoids
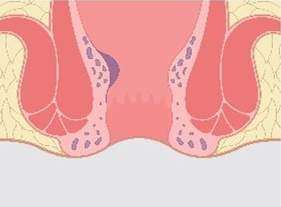
Grade 1
Internal hemorrhoids that protrude into the anal canal but do not prolapse outside the anus.
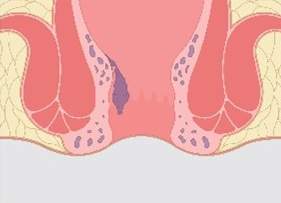
Grade 2
Internal hemorrhoids that can protrude outside the anus during straining but spontaneously return to their original internal position after straining has subsided.
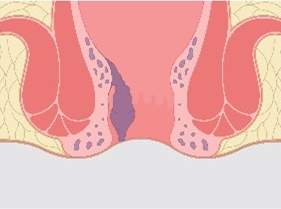
Grade 3
Internal hemorrhoids that can protrude outside the anus during straining or exertion and need manual replacement into the anal canal.
Grade 4
Prolapsed hemorrhoids which will not go back inside the anus and cause severe discomfort.
Alternative Treatments
Rubber Band Ligation
A surgeon uses a rubber band, placing it around the base of the hemorrhoid, causing the blood supply to be cut off. With no blood supply, the hemorrhoid will shrink and fall off over the next few days.
Advantages:
- Painless
- In-office procedure
- Covered by provincial insurance
Disadvantages:
- Should not be used on patients on blood thinners
- May cause excessive bleeding
- Can require multiple treatments, depending on the number of enlarged hemorrhoids
- Low Success Rate
Sclerotherapy
A chemical solution is injected into the area around the hemorrhoid, causing damage to the blood vessels feeding the hemorrhoid, which causes it to shrink.
Advantages:
- Minimal to no pain
- In-office procedure
- Quick return to everyday activities
- Can be used for individuals on blood thinners
- Covered by provincial insurance
Disadvantages:
- 4-6 weeks for hemorrhoid to shrink
- Some may experience an allergic reaction to the chemical
- Only recommended for grade 1 and 2 hemorrhoids
Excisional hemorrhoidectomy
During a traditional hemorrhoidectomy, excess tissue is removed using a scalpel, requiring sutures to close the wound. A hemorrhoidectomy is an effective treatment but can have serious side effects, including infection and incontinence.
Advantages:
- Very effective
- Covered by provincial insurance
- Can be used for both 3rd and 4th grade hemorrhoids
- Covered by provincial health insurance
Disadvantages:
- Painful
- Long recovery time
- Risk of infection
- Risk of incontinence
- Performed under anesthesia
- Risk of permanent damage to the anal canal
- Hospital stay required
Hemorrhoidopexy or stapled hemorrhoidectomy
Hemorrhoideopexy requires no incisions, and instead, staples are used to remove excess tissue and to place the prolapsed hemorrhoids back in place.
Advantages:
- Very effective
- Lower risk of infection
Disadvantages:
- Can cause a constant urge to defecate
- Can cause damage to the wall of the rectum and vaginal wall
- Cannot treat grade 4 hemorrhoids
Transanal Dearterialization of Hemorrhoids (THD)
TDH is a minimally invasive technique that uses a doppler ultrasound to identify the arteries that supply the hemorrhoid. Sutures are then used to limit the blood flow and place the prolapsed hemorrhoids back in place. The reduction in blood flow causes shrinkage of the hemorrhoid.
Advantages:
- Performed in clinic
- Lower risk of infection
- Highly effective
Disadvantages:
- Not covered by provincial insurance
- Some risk of infection